Weight Loss

Bariatric surgery or the weight loss surgery encompasses several effective procedures, namely gastric bypass, sleeve gastrectomy, gastric band, and duodenal switch. These surgical interventions have demonstrated remarkable outcomes in addressing class III obesity. Additionally, they play a crucial role in restoring metabolic balance, leading to improvements in blood sugar levels, blood pressure, and cholesterol profiles.
What is bariatric Surgery?
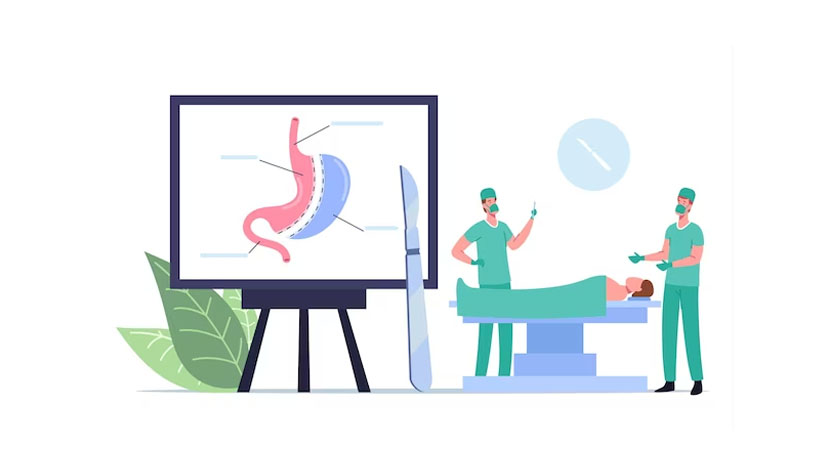
Bariatric surgery, commonly known as weight loss surgery, comprises a range of surgical procedures designed to assist individuals struggling with obesity in shedding excess weight. This surgical option is often recommended by healthcare providers when conventional weight loss methods prove ineffective, and the risks associated with obesity outweigh the surgical risks.
The primary mechanism behind bariatric surgery procedures involves altering the digestive system, typically targeting the stomach and sometimes the small intestine. By doing so, these surgeries regulate the number of calories a person can consume and absorb, leading to significant weight loss. Additionally, some procedures can suppress hunger signals transmitted from the digestive system to the brain, aiding in appetite control.
Why should we do the weight loss surgery?

Bariatric surgery stands out as the most effective and enduring treatment for class III obesity over the long term. Citing the National Institutes of Health (NIH), individuals with class III obesity face significant challenges in maintaining weight loss through diet and exercise alone. The body tends to perceive the higher weight as the new normal, triggering efforts to revert to that weight.
The essence of bariatric surgery lies in transforming the body's approach to managing food intake, paving the way for successful and sustainable weight loss alongside healthy lifestyle changes. This surgical intervention enables healthy eating habits to become more effective for achieving lasting weight loss and overall well-being.
When is the weight loss surgery advisable?
The initial step in qualifying for bariatric surgery involves confirming a diagnosis of class III obesity. This classification is determined by meeting either of the following criteria:
- Having a Body Mass Index (BMI) of 40 or higher: BMI is a measure that estimates body fat based on height-to-weight ratio. A BMI score of 40 or above indicates a substantial risk of associated health issues and typically translates to being around 100 pounds overweight.
- Having a BMI of at least 35 along with at least one related health problem: If the BMI reaches 35 and there is an obesity-related health concern, it falls under class III obesity. In the absence of an associated health problem, a BMI of 35 is considered class II obesity.
For adolescents, the eligibility requirements are somewhat more stringent. They may be considered candidates for bariatric surgery if they have:
- A BMI of at least 40 combined with an obesity-related medical condition.
- A BMI of at least 35 along with a severe obesity-related medical condition.
Although BMI can be easily determined, the diagnosis of obesity-related health conditions might necessitate undergoing specific medical tests. These tests are essential for accurate evaluation and decision-making in the context of bariatric surgery candidacy.
How is the weight loss surgery performed?
Weight loss surgery is typically carried out using minimally invasive techniques, commonly known as laparoscopic surgery. This approach involves making small incisions, leading to quicker healing, reduced pain, and less noticeable scarring compared to traditional open surgery. In most cases, laparoscopic procedures are the preferred choice for their numerous advantages.
However, it is essential to acknowledge that in rare instances, certain patients may be better suited for open surgery based on their specific medical conditions. In such exceptional cases, the surgical team may opt for the traditional open approach to ensure the best possible outcome for the patient's unique needs. Nonetheless, most weight loss surgeries are successfully performed using minimally invasive methods, providing patients with faster recovery, and enhanced overall satisfaction.
How much weight do we lose after the weight loss surgery?
Most individuals, approximately 90%, experience significant weight loss of around 50% of their excess weight following bariatric surgery, and they successfully maintain this weight loss over time. The extent of weight loss can vary slightly depending on the specific surgical procedure chosen. On average, gastric bypass surgery leads to about 70% reduction in excess body weight, while a duodenal switch typically results in an even higher percentage of approximately 80%. For sleeve gastrectomy, the weight loss outcomes range from 30% to 80% of the excess weight. These post-surgery results are typically assessed after a period of 18 to 24 months, during which patients witness notable improvements in their weight and overall health.
What are the advantages of weight loss surgery?
Significant and enduring weight loss is a hallmark of bariatric surgery, making it the most proven and effective long-term treatment for class III obesity. Beyond mere weight reduction, these surgical procedures also lead to remarkable changes in hunger hormones, promoting better appetite control and an improved metabolic profile. By rewiring the body's metabolic programming after obesity, bariatric surgery becomes the sole treatment that significantly lowers the risk of weight regain.
Moreover, weight loss surgery plays a pivotal role in managing cholesterol levels and blood sugar, often leading to remission of diabetes symptoms and enabling individuals with various metabolic syndromes to discontinue medications. The transformative impact of these procedures extends beyond mere symptom relief, contributing to an overall longer and healthier life. Scientific research has conclusively demonstrated that bariatric surgery reduces the risk of death from any cause by more than 40%, in addition to alleviating obesity-related diseases and discomforts.
Frequently Asked Questions:
Recovery times can vary depending on the type of weight loss surgery performed and individual healing rates. Generally, patients can expect to return to light activities within a week and resume normal activities within 4 to 6 weeks after surgery.
In some cases, weight loss surgery can be reversed, but it's essential to consider it a permanent procedure. Reversal may be possible for certain surgeries like gastric banding. However, it's crucial to discuss the potential risks and implications with your healthcare provider before making any decisions.
Age requirements for weight loss surgery may vary depending on the individual's health status and specific procedure. While there's generally no strict age limit, adolescents and older adults need careful evaluation to determine if they are suitable candidates for surgery.
The choice of weight loss surgery depends on various factors, including your medical history, body mass index (BMI), health goals, and lifestyle. Consulting with a qualified bariatric surgeon is essential, as they can help assess your individual needs and recommend the most suitable procedure for you.
Yes, weight loss surgery is a tool to help you achieve your weight loss goals, but long-term success relies on adopting healthier eating habits and engaging in regular physical activity. Your healthcare team will provide support and guidance to help you make sustainable lifestyle changes for lasting results.
Procedure Time:
- 2-5 hours
Full Recovery:
- 6 weeks
Anaesthetic:
• General
Back to work:
• After 2 weeks
Duration of results:
• Permanent
Results:
• Noticeable within 2 weeks
Temporary risks & complications:
• May include soreness, bleeding, persistent pain, and infection
• *Individual results and reactions may vary.
